Few pieces of exercise equipment can rival the low-impact, calorie-burning, full-body cardiovascular conditioning that the rowing machine can offer. If you don’t believe so, you probably haven’t hopped on one before. But you likely have, seeing how you’re probably hoping to get some insight on the knee pain you’ve perhaps been experiencing while using this device.
This article will walk you through all the common reasons why individuals experience knee pain with the rowing machine and what the typical path to recovery tends to look like for each of those issues.
Knee pain from the rowing machine often results from poor technique, kneecap tracking issues, reduced tissue mobility around the knee, unhealthy tendons, joint and cartilage issues, and overuse. Solutions involve using perfect technique, ensuring optimal tissue health, and proper training frequency.
Naturally, that’s just a very generalized overview of the common issues and how to fix them. If you take the time to read the rest of this article, you will learn all the juicy details and secret sauce for getting to the bottom of your pain. So, assuming you want to be enlightened, keep on reading!
ARTICLE OVERVIEW (Quick Links)
Click/tap on any of the problems below to learn why it happens and how to fix it!
• Problem 1: Poor Technique
• Problem 2: IT Band issues
• Problem 3: Muscle issues
• Problem 4: Kneecap issues
• Problem 5: Patellar tendon issues
• Problem 6: Joint-specific issues
Disclaimer: While I am a physical therapist, I am not YOUR physical therapist. As a result, I cannot tell you whether or not any treatments or training methodologies mentioned on this website or in this article may or may not be appropriate for you, including for knee pain when rowing. By following any information within this post, you are doing so at your own risk. You are advised to seek appropriate medical advice for any pain you may be experiencing.
As you read through this article, keep in mind that I can’t address every possible condition that might be driving or influencing your knee pain; numerous other conditions might be the culprit, such as Hoffa’s (fat pad) syndrome, plica syndrome, prepatellar bursitis, etc. As a result, I always advocate for a professional evaluation, whenever possible, to help interpret the underlying cause of your pain or issue.
Nonetheless, what follows are some of the most commonly experienced orthopedic issues involving the knee for active individuals and those who perform exercises involving repetitive bending and straightening of the knee, such as when rowing.
Problem 1: Poor Technique
If either or both of your knees have been giving you grief when rowing, it’s a good idea to start off by ensuring that your technique isn’t causing or contributing to the problem. The goal here is not to optimize your mechanics to maximize your athletic performance (find another article for that) — we simply want to make sure that your technique isn’t causing or contributing to why you have knee pain when rowing. In other words, just a few easy changes can make significant differences in how your knees tolerate rowing if your basic technique isn’t on point.
Check out the following technique error to ensure you’re not making any of these mistakes.
Technique error: Knock-knee positioning
One of the most common errors I see when rowing is letting the knees collapse inwards as if the knees are trying to touch one another along the body’s midline. This inwards collapsing is known as a valgus position of the knee, but it’s most commonly termed being knock-kneed.
A valgus position of the knee can lead to irritation of the knee joint, the underside of the kneecap, or the muscles and tendons crossing over the joint, especially when performed repeatedly with an activity such as rowing.
The solution for poor knee positioning
Make sure that you keep your knees stacked over your toes at all times when rowing. This ensures that your knees aren’t incurring abnormal stress and force through the joint. The knee joint is a hinge joint, which means it’s designed to work in a forwards-and-backwards plane of movement; it doesn’t tolerate sideways forces very well.
Problem 2: IT Band issues
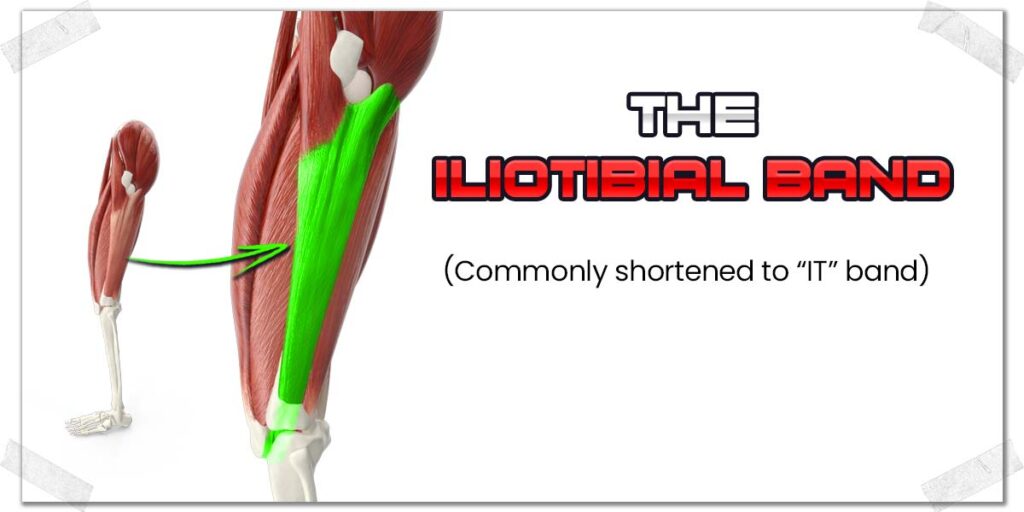
The iliotibial band (“IT band” for short) is a long, thick and fibrous band of tissue that runs down the side of the leg. It starts at the upper thigh and crosses the outside aspect of the knee, where it inserts onto the upper portion of the tibia (the shin bone).
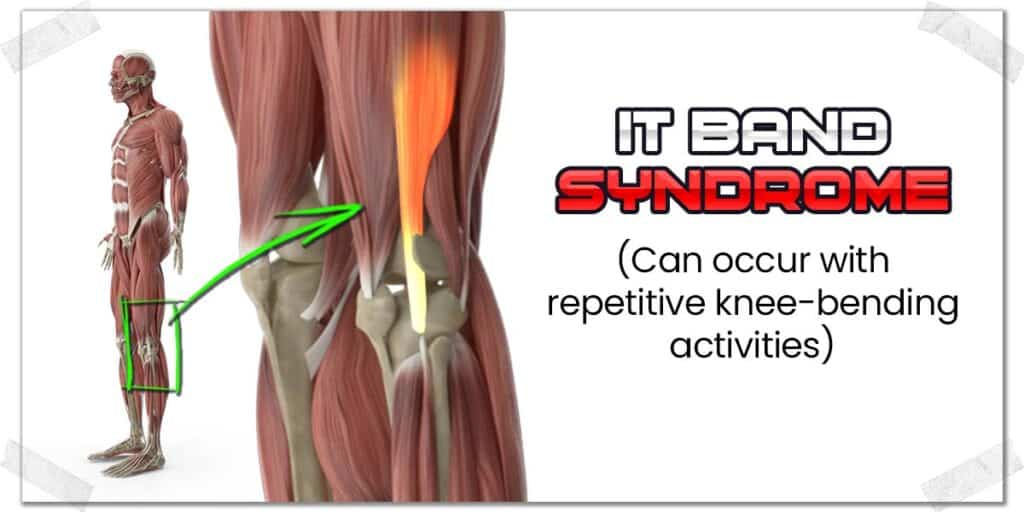
While the IT band is your best friend for assisting with hip and postural control, it can be your enemy when it’s dysfunctional, such as with IT band syndrome.
IT band syndrome is an annoying and painful condition that involves the portion of the IT band crossing over the knee becoming dysfunctional, irritated and often painful. While it’s typically seen as an overuse injury and often seen in runners, it certainly isn’t confined to this demographic; any individual who performs activities involving high repetitions of knee bending (such as rowing) can be at increased risk for this issue.1,2 It’s also seen in those who suddenly increase their overall level of physical activity.
The pain arising from the irritated portion of the IT band is primarily believed to be the result of the band being compressed over the outside portion of the knee, resulting in snapping or rubbing over the outside knob of the thigh bone just above the knee joint (known as the lateral femoral condyle).
How to treat IT band syndrome
Getting your IT band under control can take a bit of work, but it’s well worth the effort. It won’t likely be an overnight fix, but with some targeted and dedicated effort, you stand a good chance of resolving the issue and getting back to pain-free rowing.
A combined approach involving manual therapy to the IT band and strengthening specific hip muscles (the abductors) is often beneficial for those rehabbing this condition.3,4 Additionally, you may need to lay off the rowing and other repetitive knee-bending activities (such as jogging or lots of walking), depending on how irritated your IT band is.
If you want to check out some of the very in-depth details, check out this article on IT band syndrome over on physio-pedia (just make sure to come back to read the rest of this article afterwards, so you don’t miss the other important details).
Pro tip: When working on improving the tissue quality of your IT band, treat the entire band, not just the sore area. Think of the sore, bottom part of the IT band as the area where the primary car accident has occurred on the highway, and the rest of the IT band above as the road now getting backed up with traffic, creating a new host of problems.
Problem 3: Muscle issues
There are a handful of muscles that cross over the knee joint, which are responsible for bending and straightening the knee. Anytime these muscles are tight, immobile or otherwise unhealthy, it can influence how the knee moves or the pain that we may feel within the knee region. What follows is a brief list of muscles that, when not healthy to a certain extent, can cause the sensation of knee pain when rowing:
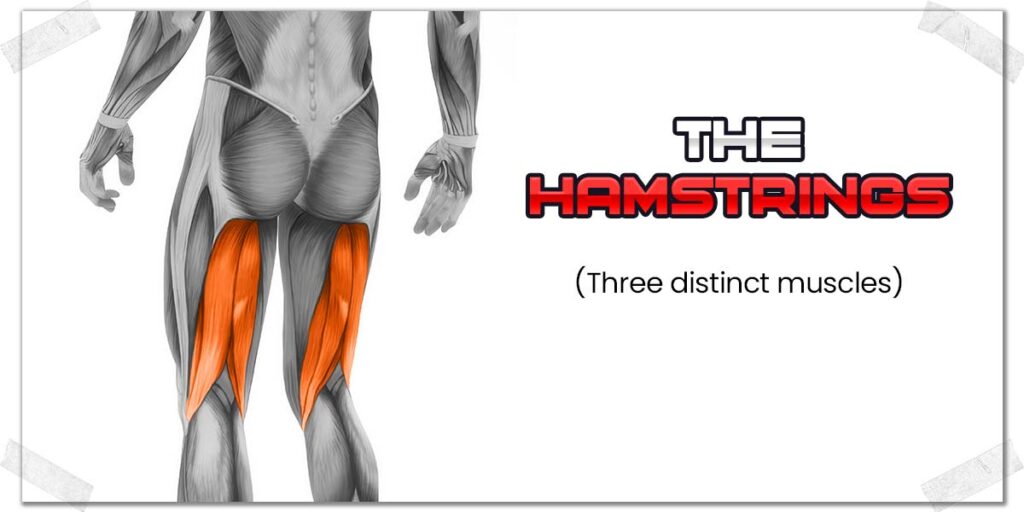
The hamstrings
The hamstrings are a group of three different muscles on the back of your thigh, which cross the knee joint. When these muscles contract, they bend the knee. In the context of rowing, they also help you straighten your knee at a controlled rate (i.e., a controlled lengthening of the muscles), which is known as an eccentric contraction.
Due to the knee-dominant nature of the rowing machine, the hamstrings receive high levels of use. If these muscles are tight, immobile or even lack the endurance to make it through the demands of your rowing session, they can become uncomfortable, producing sensations of tightness, discomfort or even pain.
Keeping your hamstrings healthy, strong, and supple should always be a top priority in your training, no matter what type of training you perform. It will save you a world of pain and disability by keeping your low back, hips, and knees.
Solutions for your hamstrings
If your hamstrings are the culprit for your knee pain when hopping on the rowing machine, you’ll need to determine if the pain is from generalized tightness (immobility of the muscles) or if it’s from another issue, such as tendinosis (which is beyond the scope of this article).
If you need to improve and optimize the mobility of your hamstrings, here are some generalized starting points to consider:
- Don’t perform crazy-intense stretching; your muscles will likely respond better to lower intensity stretches with high frequency (multiple times per day). Aggressive stretching might only make your discomfort worse.
- Consider incorporating hamstring strengthening exercises into your training. It sounds counterintuitive, but there’s good evidence to show that muscles can be abnormally tight due to a lack of strength.5
- Using a heating pad or other heating device can be an effective way to relax the hamstring muscles while decreasing tension-related discomfort in the process. Consider putting heat on the tight or sore area before a workout and at other points throughout your day.
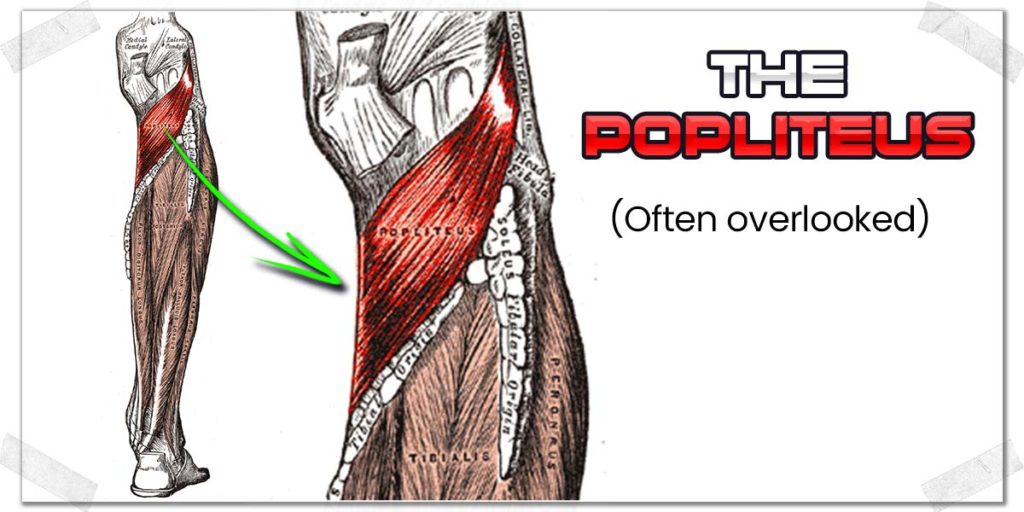
The popliteus
The popliteus is a not commonly known but all too common culprit for knee pain. This sneaky little muscle sits on the backside of the knee joint and is buried beneath every other muscle on the back of the knee. Its primary responsibility is to help initiate knee bending movements.
Unfortunately, this little guy has the propensity to become tight, which can lead to sensations of discomfort behind the knee, most notably when the knee is entering its final few degrees of achieving full extension (straightening of the joint).
Solutions for your popliteus
Since the popliteus is such a deep muscle, it can be a bit tricky to treat. However, a skilled orthopedic physical therapist can give it some love and care, for sure. If seeing a professional is not in the cards for you, giving it some deep, sustained pressure with your thumbs will likely be your best bet. To learn more, check out my article:
Pain Behind Your Knee When Squatting? Causes | Fixes | What to Know
Pro tip: Since the sciatic nerve, tibial artery, and tibial vein all run right down the middle of the popliteus, you don’t want to press in this area; press off to either side to avoid irritating the back of your knee.
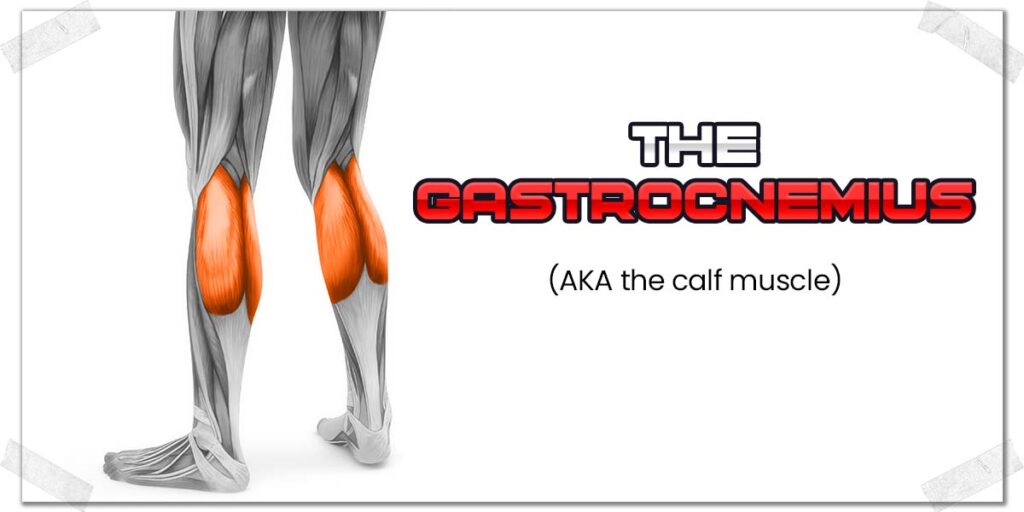
The gastrocnemius
The gastrocnemius muscle — most commonly known as the calf muscle — is the incredibly popular muscle on the back of the lower leg that everyone knows. It’s what gives the shape to this portion of the lower leg. It consists of two muscle heads that originate above the knee joint and insert onto the heel bone (the calcaneus) via the Achilles tendon.
Since the gastrocnemius crosses the knee joint, it acts as a very weak knee flexor muscle. As a result, dysfunction (tightness, weakness, etc.) within the muscle can lead to pain or discomfort within the knee region, most often on the lower backside of the joint.
Solutions for your gastrocnemius
There are plenty of ways to give your gastrocnemius muscle(s) some self-treatment if you’re not keen on getting a professional to treat you. I’ve written an entire article on how to do so. If you want the details, check out my article:
The Seven Best Way to Massage Your Calf Muscles All By Yourself
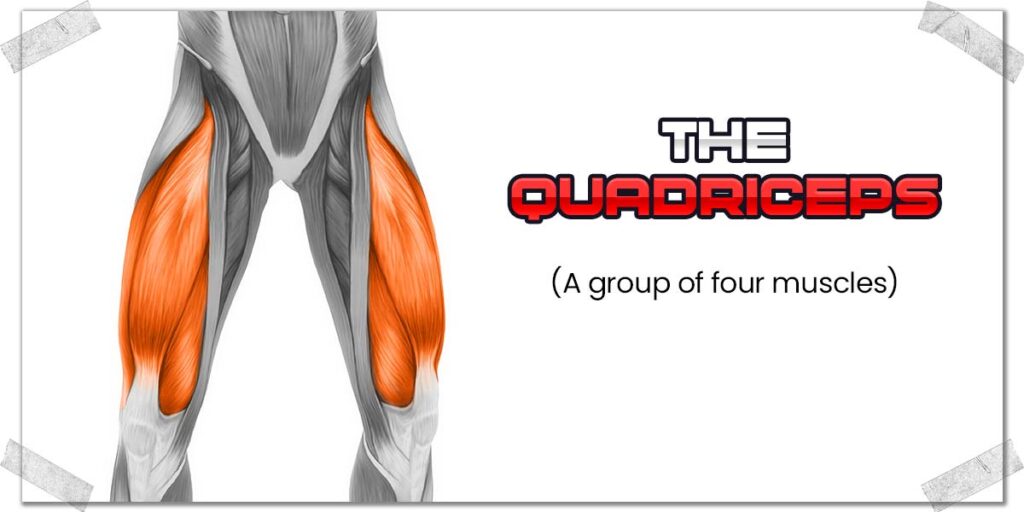
The quadriceps
Tightness within the quadriceps muscles — while not normal — is rather common in individuals, especially those who are regularly physically active. If these muscles have enough chronic tension within them, it can produce sensations of discomfort or pain around the front of the knee (most notably when the rectus femoris muscle is tight).
Pro tip: This phenomenon is known as referred pain — where pain arising in one area of the body is felt or perceived in another area.
A second complication that can arise is altered (reduced) mobility of the kneecap, where the kneecap can’t move as freely as necessary when performing knee bending movements. This will be expanded on a bit more in the following section.
Solutions for your quadriceps
If your quadriceps muscles are feeling rather tight or loaded up with some sensitive spots when you press on them (known as trigger points), giving them a bit of love and care to restore mobility and relieve tension can be a great starting point.
Common ways of improving your quadriceps mobility and decreasing muscle tension include:
- Foam rolling
- Massage therapy
- Heat
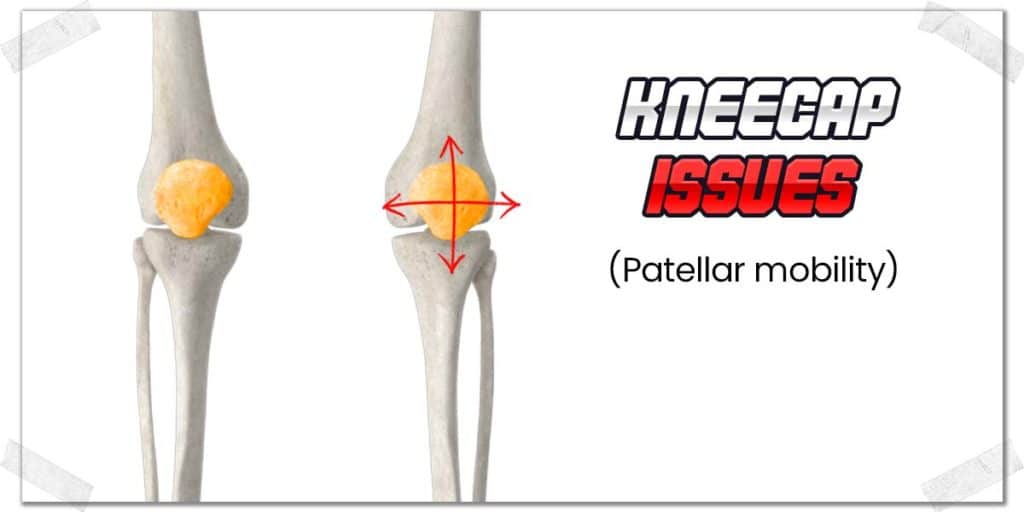
Problem 4: Kneecap issues
A kneecap (the patella) tracking issue is one of the more common knee issues that can result when muscle tissue around the thigh and knee are tight, restricted, and otherwise not as supple as ideal.
The patella itself is actually encased within the tendon that attaches the quadriceps muscles to the shinbone. As a result, the kneecap position (and its ability to move) depends on the overall mobility of quadriceps muscles and its common tendon.
Normally, the underside of the kneecap sits perfectly in a little groove (known as the intercondylar notch of the femur), allowing the backside of the kneecap to glide perfectly within this groove.
If the kneecap can’t sit perfectly within this groove, it can lead to abnormal tracking and subsequent irritation of the cartilage on the underside of the kneecap. This condition is known as patellofemoral syndrome.
Related article: Tight Kneecap? Get it Moving with These Techniques (Way Less Pain)
These tracking issues can arise for a couple of common reasons:
- Muscular weakness from the inner quadriceps muscle (known as the vastus medialis).
- Tight or restricted outer thigh tissue, such as the vastus lateralis muscle, the lateral retinaculum, and the IT band.
- A combination of both factors described above.
How to fix patellar tracking issues
The best approach for improving your patellar tracking is to start by getting a professional assessment to determine the underlying cause of the tracking issue. However, if getting a professional assessment isn’t in the cards for you (for whatever reason), a combined approach involving strengthening the inner quadriceps and mobilizing the muscles and tissues on your outer thigh will likely be of benefit.
As a starting point, if you want to learn about my favorite home exercise for specifically strengthening the inner quadriceps, check out my article:
Activate & Strengthen Your VMO With This Science-proven Exercise
When it comes to helping to restore the mobility of the outer thigh muscle and IT band, some self-treatment techniques that have been shown to be effective include:
- Foam rolling
- IASTM
- Voodoo flossing
If appropriate for you, implement one or more of these self-treatment techniques on a daily basis and do so for a few weeks in a row. Chances are, by then, you’ll notice a reduction in your knee pain symptoms if your pain is the result of a tracking issue due to tight outer thigh tissue.
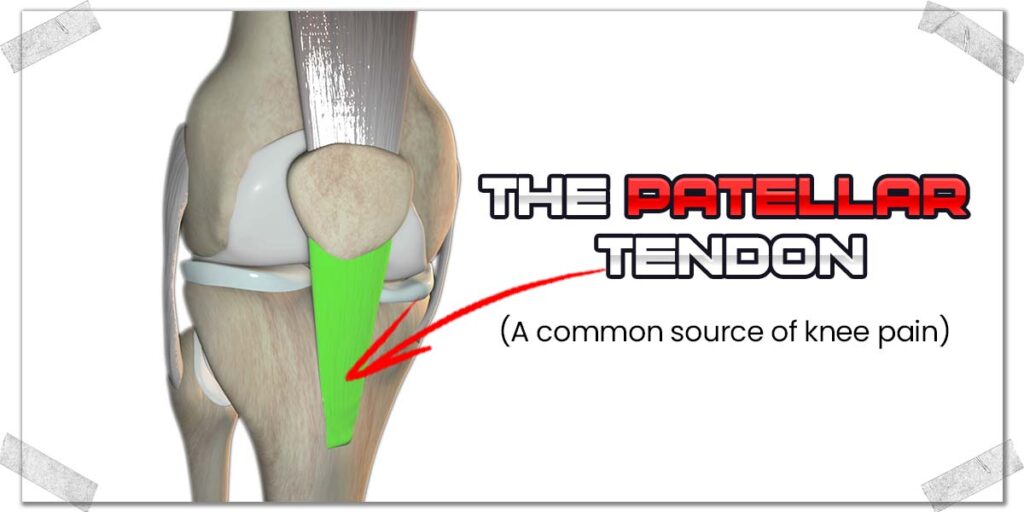
Problem 5: Patellar tendon issues
The patellar tendon refers to the thick, gristly piece of tissue that runs from your kneecap and anchors down onto the top of the tibia (shin bone). Due to how much repetitive work and force this tendon must undergo, it’s not uncommon for it to become sore, painful, and unhealthy.
The most common conditions involving the patellar tendon include:
- Patellar tendonitis
- Patellar tendinosis
For the record, the terms patellar tendonitis and tendinosis are often interchanged. Still, they are technically different conditions and require different treatment strategies as a result.
Regardless of whether the issue is tendonitis or tendinosis, the underlying mechanism that tends to bring on either condition is repetitive movements that exceed the capacity of what the tendon can tolerate. This is known as a repetitive strain injury (RSI).
Since rowing involves repetitive movement of the knee joint while simultaneously placing a load (resistance) through the tendon, the risk of incurring a repetitive strain injury for the tendon can be relatively high for specific individuals.
Overcoming patellar tendonitis and tendinosis
Any time a tendon is irritated or chronically unhealthy, you need to be smart and calculated with getting things back under control and up to full health. An entire series of blog articles could be written on this topic (I’m working on it).
In the meantime, here are the starting points for dealing with this issue:
- Tendon injuries don’t heal up entirely just with rest; they need to be stimulated with exercise that doesn’t worsen the pain.
- Movements that stimulate the tendon should be performed with very slow and controlled movement.
- Stick with resistance levels that generate a slight sense of effort with a minimal ache (but not pain).
- Opt for performing around three sets of ten repetitions once per day.
- You’ll likely want to forego intense, aerobic exercises (such as fast-paced rowing) until the tendon is back to full or optimum health.
Related article: Spanish Squats for Patellar Tendinopathy How | Why | When (Must Know)
Problem 6: Joint-specific issues
There can certainly be a handful of issues that can arise from within the knee joint itself, all of which can create pain and dysfunction. For this article, I’ll very briefly point out a few common potential issues, which will hopefully help point you in the right direction for learning about these conditions.
For the most common condition (osteoarthritis), I’ll be diving into that one a bit more specifically.
Some joint-specific issues causing knee pain when rowing include:
- Plica syndrome
- Meniscal injury
- Ligamentous injury
- Joint mice
Osteoarthritis of the knee
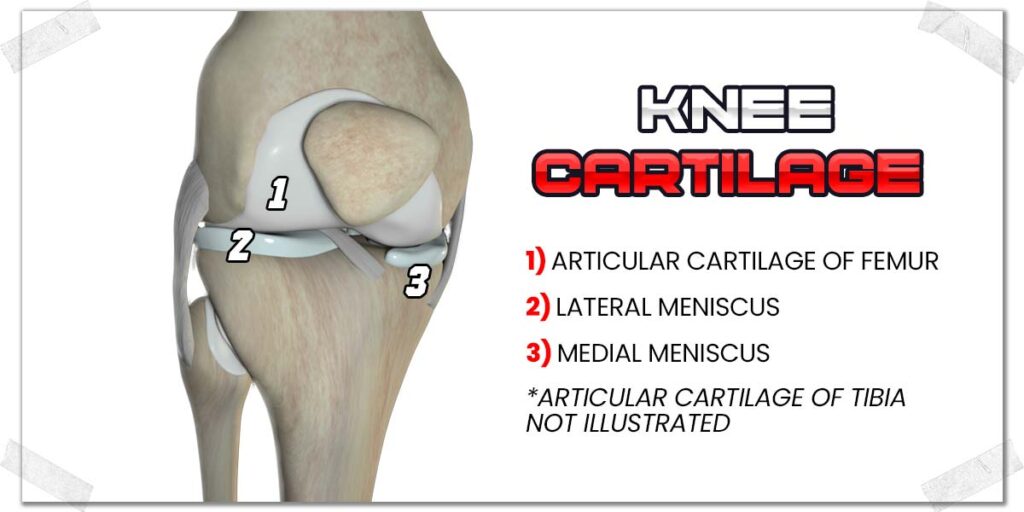
Osteoarthritis refers to the breakdown or destruction of articular cartilage between the ends of two bones (in this case, the tibia and femur bone). It is a rather common condition in the aging population around the world, with its onset most often appearing in individuals within their fourth and fifth decade of life.6
As the smooth cartilage surface(s) breaks down, the articulation of the joint is no longer smooth, resulting in irritation and pain within the joint. It tends to affect the inside portion of the knee (the medial aspect) the most, though this isn’t always the case.
Depending on how arthritic the joint is, the strategies required to alleviate the issue vary greatly. Nonetheless, what follows below are some general considerations and strategies that can often be useful for arthritic knees.
Also, you may be able to continue rowing if your knee pain is purely from arthritis; however, you will need a professional evaluation from a qualified practitioner to determine if it’s safe to do so. Some individuals need to alter (lessen) their resistance, range of motion, or overall exercise intensity on the rower. In doing so, they find that their knee pain is not worsened during rowing. Ultimately, it all depends on how advanced the arthritis within the knee may or may not be.
Strategy 1: Keep the knee moving
Arthritic knees tend to be a bit of a balancing act — if you keep them still all the time, it can make things worse. Conversely, if you are too aggressive with movements, it can also irritate the joint.
Generally speaking, finding movements and activities that don’t cause pain to worsen is a wise idea. Common activities that can be tolerated well include:
- Stationary bike riding (upright or recumbent)
- Aqua therapy/water aerobics
- Knee slides (while sitting or laying on your back)
Strategy 2: Strengthen your hip
The muscles of the hip help to significantly control and assist the positioning of the knee joint itself. The weaker your hip muscles are, the more your knee will likely collapse inwards, twist, or generally wobble around. With an already unhealthy knee joint, the last thing you want is to put further stress and strain on and through the joint by adding rotational instability from the hip.
The key muscles you’ll likely want to target for helping to control the stability of your hip (and thus, your knee) are:
- The glute medius
- The glute minimus
- The tensor fascia latae (the TFL)
Pro tip: The glute medius and minimus muscles essentially work together, so any exercise you incorporate to strengthen the glute medius will also strengthen the glute minimus and vice versa.
There are, naturally, other muscles that could be of benefit (including the glute maximus); however, starting with finding exercises for the muscles above would be a fantastic starting point.
Related article: The Best Glute Medius & Minimus Exercise That No One Is Showing You
Final thoughts
Your knees are too precious to ignore if they’re in pain, and the rowing machine is too great of a tool to forego if you can help it. So, take the insight within this article and use it to help point you in the right direction for getting things under control. Be smart, be patient, and be determined to do all that you can to get to the root cause of the issue so you can get back on track with your rowing.
References:
3. Themes UFO. Deep Dry Needling of the Hip and Pelvic Muscles. Musculoskeletal Key. Published October 7, 2019. Accessed May 19, 2022. https://musculoskeletalkey.com/deep-dry-needling-of-the-hip-and-pelvic-muscles/
6. Knee Osteoarthritis. Physiopedia. Accessed May 5, 2022. https://www.physio-pedia.com/Knee_Osteoarthritis

Hi! I’m Jim Wittstrom, PT, DPT, CSCS, Pn1.
I am a physical therapist who is passionate about all things pertaining to strength & conditioning, human movement, injury prevention and rehabilitation. I created StrengthResurgence.com in order to help others become stronger and healthier. I also love helping aspiring students and therapists fulfill their dreams of becoming successful in school and within their clinical PT practice. Thanks for checking out my site!