NOTE: If you’re looking for a complete introduction pertaining to blood flow restriction training, including when, how and why to use it, be sure to check out my article: What is Blood Flow Restriction Training? How, Why and When to Use it as it contains a complete rundown on everything you need to know.
This article will comprise some basic information on blood flow restriction for clinical populations that I’ve gathered through intensive research in academic literature (over the last two years) as well as through my own anecdotal experiences on my patients within the clinic.
If you’re looking for the quick takeaway on the evidence for blood flow restriction, for clinical populations, here it is:
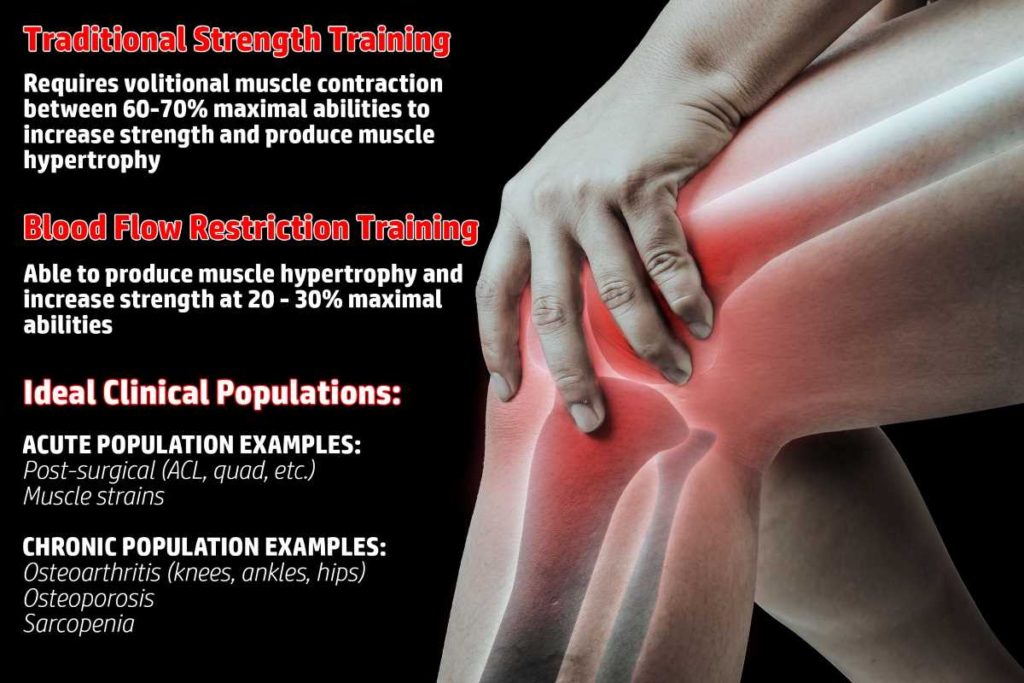
Blood flow restriction has been shown to have very favorable and effective outcomes in increasing muscle strength and size with individuals who have specific acute or chronic musculoskeletal issues within their body. It can be a highly effective adjunct in the rehabilitative setting when used appropriately.
Literature has shown favorable findings for conditions such as post-surgical ACL reconstruction, patellar tendonitis, osteoarthritis of the knee and generalized sarcopenia. More literature is warranted for further understanding the effects of BFR on these musculoskeletal pathologies, but evidence at this time suggests that BFR is capable of reducing rehabilitation time (and pain, in some conditions) while maximizing muscle hypertrophy and strength throughout the process.
As I present information within this blog post, I am assuming that you have a basic understanding as to what blood flow restriction training/therapy consists of as well as how it’s typically performed. If not, please check out my article: What is Blood Flow Restriction Training? How, Why and When to Us it to read up on all the details.
The aim of this article is not to promote superiority of this intervention over others; the aim is to give insight as to why it can be considered a promising new tool in the therapist’s toolbox of rehabilitative interventions.
A quick overview of this article
- Why choose to implement blood flow restriction into clinical practice?
- Evidence for enhancing muscle hypertrophy and strength in acutely injured populations
- Evidence for chronic populations & elderly populations (osteoarthritis, osteoporosis & sarcopenia)
- Walking protocols
- Evidence for pain reduction
- Concluding remarks
Each one of these topics is discussed in further detail below, so be sure to keep reading!
Also, if you’re curious as to which BFR cuff system I recommend (and personally use on myself and my patients), head over to the My Recommendations page, where you’ll get a detailed breakdown on the system that I recommend. You can also receive a 10% discount with a coupon code I’ll give you.
Why choose to implement blood flow restriction into clinical practice?
When it comes to implementing a musculoskeletal (MSK) rehabilitation intervention for their patients, physical therapists have no shortage of modalities and protocols to choose from (some effective, some not so effective). Every intervention the therapist uses must be preceded by sound clinical reasoning and take into account the unique factors and circumstances for that particular patient. Utilizing blood flow restriction therapy is no different.
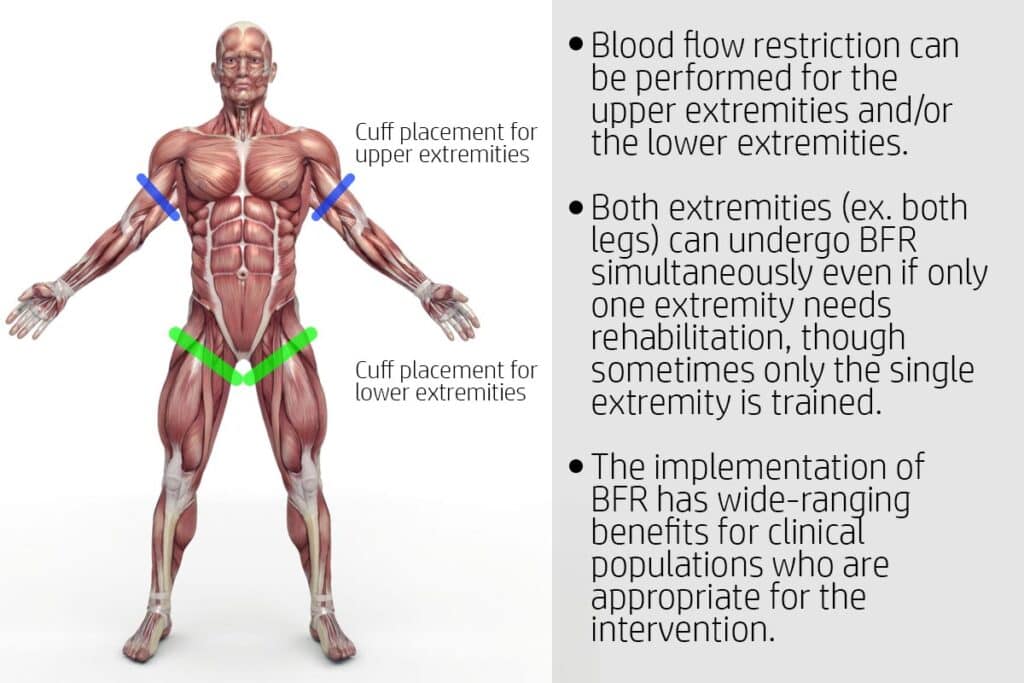
When appropriate to implement, blood flow restriction holds many unique benefits for improving muscular strength, endurance and hypertrophy (cross-sectional area) of the limbs (either for the upper or lower extremities). Certain clinical practices and physical therapists with specialties in orthopedics deal with a primary patient caseload who are at increased risk of muscular atrophy and/or strength loss. This can be due to acute injuries or chronic pathologies (diseases) incurred by the patient. When loss of strength and muscular endurance occur to enough of an extent, these patients also experience secondary issues of pain and reduction in functional abilities.
Therefore, an intervention that can minimize or even reverse this process due to early and repeated implementation of an overload stimulus to the muscles is critical. However, this stimulus must be delivered without causing undue pain to the patient or overly stressing any compromised tissues. This is exactly where blood flow restriction for therapeutic rehabilitation comes in.
These populations can be prime candidates for BFR therapy and its subsequent rehabilitation protocols. To read more on BFR protocols, head on over to the article I mentioned at the top of this post.
Unique advantages to implementing BFR for MSK rehabilitation
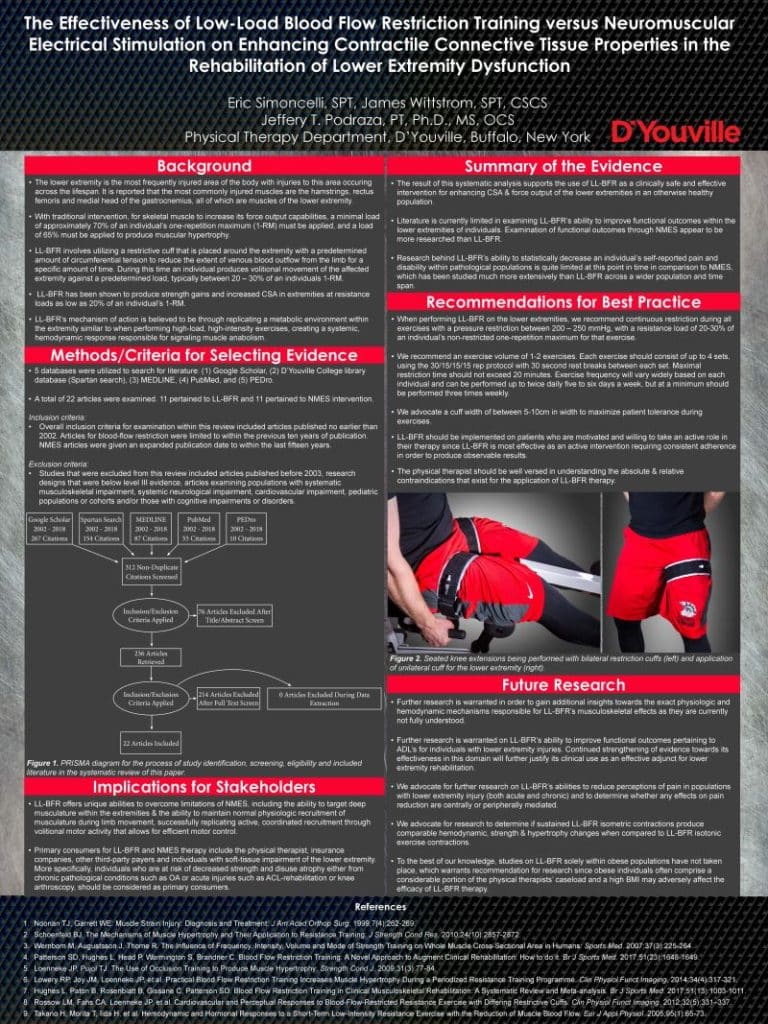
Since BFR is an active intervention (i.e. the patient must perform volitional work), it houses some unique benefits over traditional muscle strengthening modalities such as neuromuscular electrical stimulation (NMES), which is largely a passive intervention.1,2
While BFR can be used passively (i.e. just put the cuff on and the patient sits passively throughout out its application), the studies I’ve come across tend to show much better results when its utilized with active movements (even something as simple as isometric contractions or short-arc quad sets).
I’ll briefly highlight three unique benefits that BFR houses over more traditional electrotherapy modalities and interventions. Electrotherapy (electrically stimulating a muscle in order to contract) is a traditional modality that therapists often use when trying to increase strength for an extremity that is too weak or painful to load through traditional resistance training protocols.
- Targeting deeper musculature
- More natural and more efficient motor unit recruitment patterns
- Psychological benefit to the patient
Targeting deeper musculature
While NMES is often used to stimulate muscles of an injured limb (in attempts to re-gain strength, prevent atrophy, etc.) one of the shortcomings of this intervention is its inability to effectively target deeper musculature underneath the more superficial musculature.3 This is due to the fact that the electrical current from surface electrodes must always pass through superficial muscles, thus these superficial muscles receive ample stimulation while deeper muscles may not be as adequately stimulated.
As an example, if attempting general quadriceps strengthening exercises as a means to improve walking abilities, knee extension, etc., BFR theoretically could improve muscle strength and hypertrophy to the deeper vastus intermedius to the same extent as within the more superficial rectus femoris, vastus medialis and vastus lateralis.
More natural and more efficient motor unit recruitment patterns
Another unique benefit of BFR is its ability to improve strength and muscle size without altering the body’s normal motor unit recruitment patterns. This is due to the fact that BFR is an active intervention, so the volitional movement and motor unit recruitment patterns produced by the patient are no different than if they were performing the volitional movement without BFR.
Contrast this with an attempted strengthening intervention such as NMES and it becomes an entirely different story. NMES will stimulate whichever muscles the electrical current is being driven into (i.e. the muscles that are closest to the electrodes get the most input while muscles further away get the least input). Aside from this producing a much less natural movement pattern/order of muscle recruitment, it also tends to be a much less mechanically efficient recruitment pattern as well when compared to the body’s own natural recruitment strategies.1
None of this is to say that an intervention such as NMES can’t improve strength, prevent atrophy, etc. NMES has long been studied and has found to be able to increase muscular strength within extremities. Rather this is to highlight the fact that BFR holds some unique advantages over a more traditional strengthening intervention for injured populations.
Psychological benefit to the patient
This particular benefit of BFR is completely anecdotal based on my own experiences, so keep that in mind. Nonetheless, I feel it can be incredibly valuable for certain types of patients.
I’ve found that there are particular types of patients who, when unable to contract the muscles in their arms or legs to higher levels of exertion (due to pain, post-surgical healing limitations and timelines, etc.), can feel rather frustrated. This frustration arises from their inability to challenge their limbs in a way that produces the feeling of higher levels of exertion or muscular fatigue – the feeling that they associate with hard work and progress.
BFR can counter this by producing enough physical fatigue within the extremities to the point that it results in the patient feeling they had to really exert/challenge themselves to complete their exercise(s) (all without undergoing higher mechanical loading or intensity). This perception of high levels of effort and subsequent fatigue helps the patient feel that they’re challenging themselves enough to produce favorable increases in strength and endurance.
This tends to be in patients who are more active and fearful of regressing in their current abilities, but I’ve seen it enough that it’s worth mentioning. When patients have the ability to perform an exercise intervention for which they feel they have to work rather hard at while simultaneously feeling the resulting muscle fatigue, they tend to enjoy therapy more. They also tend to fully buy into the intervention and have less perceived helplessness when recovering from their injury or condition as well.
Evidence for enhancing muscle hypertrophy and strength in acutely injured populations
When it comes to the evidence for BFR increasing muscle hypertrophy (size) within clinical populations, the evidence is favorable. Acutely injured clinical populations can be those recovering from surgical interventions (ACL reconstruction, meniscectomy) or tendon-based pathology such as tendinitis/tendinosis.
Following a musculoskeletal injury, it’s important to appropriately load (and thus stimulate) tissues within the extremities as soon as appropriately possible. This is well understood in the world of physical rehabilitation when it comes to reducing or preventing muscular atrophy and/or strength & power loss. The quicker muscle, bone and tendon can be stimulated, the less atrophy, loss of strength and range of motion the individual is likely to experience.
When looking at meta analyses (systematic reviews) along with randomized controlled trials (RCTs) within the literature, there continues to be growing evidence for the efficacy of BFR as an effective intervention for these individuals. ACL reconstruction is perhaps the most widely studied lower extremity post-surgical condition regarding the use of BFR for rehabilitation. Statistically significant findings in strength and/or muscle hypertrophy have been found with a variety of patient populations when implementing various protocols.4,5
There are also case-study reports (lower level of evidence than RTCs) that show favorable outcomes in patients who have patellar tendonitis and osteonecrosis of the medial femoral condyle, osteochondral fracture and knee arthroscopy.6–9 While these are case study reports, the favorable outcomes warrant mention (along with further study regarding BFR on these conditions).
Evidence for chronic & elderly populations (osteoarthritis, osteoporosis & sarcopenia)
With elderly populations being at increased risk for conditions such as osteoarthritis and generalized sarcopenia, blood flow restriction therapy has been a hot topic of study for many researchers. Any intervention that holds the potential to allow for muscle and strength increase while reducing or avoiding pain provocation or worsening of symptoms warrants scientific study.
Research has found significant, favorable findings for improving strength for women with symptomatic knee osteoarthritis, women with osteoporosis, and for allowing men with osteoarthritis of the knee to perform resistance training without any worsening of pain when compared to their respective control groups.10–12 Studies involving walking protocols (discussed later within this article) for elderly populations have also been conducted and have shown statistically significant increases in low extremity strength over their control group.13
Elderly populations within these studies who performed resistance training (i.e. not a walking protocol) performed BFR training anywhere from 2 – 4 times per week for 5 – 12 weeks. This should serve to remind the clinician and patient that intervention involving BFR training needs to be performed consistently for a sustained period of time in order to elicit favorable and noticeable responses.
Pain reduction
Pain reduction has been reported in subjects who underwent BFR training, though this is not a universal finding across all studies. For populations with symptomatic knee osteoarthritis, outcome measures tend to be reported through the Knee Osteoarthristis Outcome Score (KOOS), the Veterans RAND 12-item Health Survey (VR12) or the Western Ontario & McMaster Universities Osteoarthritis Index (WOMAC).
Walking protocols
Aside from performing resistance training exercises, BFR has also been used (and shown to be effective) with regular walking. Though this method or type of exercise is different than when compared to resistance/strength training protocols, the application and delivery of the BFR intervention itself is unchanged; patients place the restrictive cuff(s) just beneath the gluteal fold with appropriate pressure and then proceed to walk continuously for upwards of twenty minutes.
These walking protocols have been shown to improve functional outcomes in those with osteoarthritis of the knee while simultaneously improving strength and muscle hypertrophy within the lower extremities. Protocols have varied within literature but tend to have the subjects perform their walking protocol anywhere from 2-5 times per week for upwards of 10 or more weeks.
Walking protocols could therefore be a very reasonable approach to patients and individuals who are looking to maintain their general fitness, improve strength and function within their legs and doing so without the need for specific exercise equipment.
Concluding remarks
Blood flow restriction continues to gain evidence within scientific literature and traction within clinical practice. Its potential applications towards a particular demographic of patients should pique the interest of practitioners who work with this clinical population as it offers the ability to make resistance training exercises more tolerable to certain individuals while simultaneously improving functional outcomes, muscle strength and hypertrophy.
Though more research is warranted for multiple aspects of its clinical applications (specifically for specific types of musculoskeletal and orthopedic conditions), evidence is showing that it is a promising intervention for reaching clinical populations who cannot tolerate heavier resistance loads or higher intensity movements when trying to maintain or improve strength, hypertrophy and functional abilities within the extremities.
If you’re considering picking up a professional pair of BFR cuffs for either yourself or for your clinic, my personal recommendation is the BSTRONG system. The cuffs hold up well, are designed by a medical team and won’t break the bank when purchasing. Head on over to my recommended BFR page, where you can get a coupon code to get 10% off any of your BSTRONG purchases.
Works Cited
2. Kramer JF, Mendryk SW. Electrical Stimulation as a Strength Improvement Technique: A Review. J Orthop Sports Phys Ther. 1982;4(2):91-98. doi:10.2519/jospt.1982.4.2.91

Hi! I’m Jim Wittstrom, PT, DPT, CSCS, Pn1.
I am a physical therapist who is passionate about all things pertaining to strength & conditioning, human movement, injury prevention and rehabilitation. I created StrengthResurgence.com in order to help others become stronger and healthier. I also love helping aspiring students and therapists fulfill their dreams of becoming successful in school and within their clinical PT practice. Thanks for checking out my site!